Case Report:
Soren is a 4 year old, male neutered, German Shepherd Dog.
History:
Presented to ER after his owner picked him up from doggie daycare and noted he seemed lethargic, vomited twice, and ulcerations were seen on his tongue.
Initial physical exam and diagnostics:
- Initial physical exam revealed a fever of 103.8 F, bleeding ulcerations on the periphery of the tongue, and mild hypersalivation.
- CBC was unremarkable.
- Chest x-rays did not have any significant findings.
Initial differential and plan:
Electrocution was the initial differential given the acute onset of signs, physical exam findings of mouth ulcerations, and the fact that he had been at daycare. Other possible differentials at that time included ingestion of a caustic substance, vasculitis, and neoplasia.
The recommended plan was monitoring in the hospital overnight for signs of electrocution (non-cardiogenic pulmonary edema) and GI supportive care for the few episodes of vomiting.
Initial treatments:
- Sucralfate PO every 8 hours as a slurry
- Maropitant as an antiemetic
Day 2 physical exam and diagnostics:
Soren was persistently febrile, the ulcers appeared progressive from the prior day, and the tongue was now moderately diffusely swollen, making it difficult for him to close his mouth. New erythema was noted on the ventrum extending up towards the axilla; fur was shaved to more closely monitor this. He also developed bilateral blood-tinged, mucoid nasal discharge.
Chest x-rays were repeated to monitor for signs of NCPE in case this was due to electrocution, and they revealed a “progressive ventral pulmonary infiltrate likely reflecting pneumonia” with a distribution not typical for NCPE.
A chemistry panel was performed and had no specific findings.
Updated differential and plan:
Electrocution was considered less likely given the progression of the ulcerations, new skin findings, and lack of NCPE. The doggie daycare also was contacted and confirmed there was no access to any cords or electrical source.
An updated differential list for the constellation of symptoms now favored interaction with a caustic substance (via ingestion and topically given the skin lesions) or vasculitis. The fever was considered likely multifactorial from the pneumonia and inflammation surrounding the ulcerations and skin. The pneumonia was considered likely aspiration from the few episodes of vomiting prior to presentation.
A vector-borne disease panel and testing for leptospirosis were submitted to look for possible infectious diseases causing vasculitis.
Updated treatments:
- Fluids (lactated ringers) were added due to decreased appetite and inability to drink efficiently at 45 ml/kg/day.
- Unasyn was added due to concern for aspiration pneumonia.
- Magic mouthwash (3 parts Carafate, 1 part Nolvadent, 1 part Lidocaine 2% injectable).
- Pantoprazole was added to treatments due to concern for possible ingestion of a caustic substance and GI ulceration.
- Maropitant and sucralfate were continued.
Day 3-7 of hospitalization:
Due to persistent fever, lack of appetite, and progression of tongue swelling/ulcerations, Soren remained hospitalized for several days for supportive care. He was interested in food and attempted to eat and drink but would often drop food or go to ingest something and then stop. We began offering food in a slurry form, which seemed to help him eat. No further vomiting was seen during hospitalization.
The tongue swelling improved and nearly resolved after ~3 days. The ulcerations stopped progressing and remained static. Soren’s respiratory rate and effort were closely monitored, he remained eupneic on room air and did not require oxygen supplementation. He did have a productive cough. His energy level improved, and his personality became more playful and interactive. Due to persistent fever and cough on Day 6, chest x-rays were repeated and showed a more severe ventral alveolar infiltrate due to progressive pneumonia.
His nasal discharge remained static for about 3 days, then started to improve. It remained thick, blood-tinged, and mucoid.
Treatment changes:
- Gabapentin was added for additional analgesia.
- Enrofloxacin was added to expand the spectrum of bacteria treated for his pneumonia.
- Entyce was added as an appetite stimulant.
- Pantoprazole IV was transitioned to omeprazole PO.
- Unasyn IV was transitioned to Clavamox PO.
- Maropitant, Sucralfate, and Magic Mouthwash were continued.
Discharge and update:
Soren was discharged after 7 days of hospitalization. He went home taking omeprazole, sucralfate, clavamox, enrofloxacin, magic mouthwash, and gabapentin, all by mouth. His appetite had improved, and he was able to comfortably eat soft food. His cough and nasal discharge persisted for about 1 week then resolved. Soren’s ulcers completely resolved after about 2 weeks. His skin erythema developed into dry lesions that healed around the same time frame.
Conclusions:
Soren’s infectious disease testing all came back negative. Given his constellation of signs, the most likely diagnosis is interaction with a caustic substance, likely a cleaning bleach solution used at the doggie daycare. It is thought that he licked some of the cleaner as well as laid in it causing the tongue ulcerations and skin erythema. It is possible the nasal discharge was either due to the pneumonia or damage to the sinuses if any of the nasal passageway was exposed to the caustic substance.
Caustic substances can be either acidic or basic, and both types can cause significant injury. They can cause ulceration of the GI system, oral mucosa, and skin if contacted. This can be limited to the mouth if just licked or extend to the esophagus/stomach if ingested. Injuries can range from mild to severe and corrosive. Worst case scenario can involve ulcers of the GI system that perforate or the development of an esophageal stricture.
Examples of alkali substances include:
- Bleach
- Dishwasher detergent
- Batteries
- Drain cleaner
- Oven cleaner
- Hair relaxer
Examples of acidic substances include:
- Toilet bowl cleaner
- Sulfuric acid
- Hydrochloric acid
- Metal cleaners
- Pool sanitizers
- Batteries
 Close-up view of a dog’s belly showing red, irritated skin with signs of swelling and fur loss in the central area.
Close-up view of a dog’s belly showing red, irritated skin with signs of swelling and fur loss in the central area.
 Image of a dog’s open mouth with visible tongue ulcerations along the edges, showing signs of redness and irritation.
Image of a dog’s open mouth with visible tongue ulcerations along the edges, showing signs of redness and irritation.
 Close-up of a dog’s tongue showing pronounced ulcerations and redness, particularly at the tip and sides.
Close-up of a dog’s tongue showing pronounced ulcerations and redness, particularly at the tip and sides.
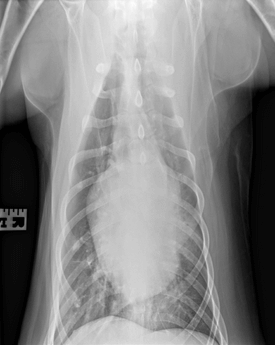 X-ray of a dog’s chest taken from a frontal view, showing lung and heart structure with some indications of possible infiltrates.
X-ray of a dog’s chest taken from a frontal view, showing lung and heart structure with some indications of possible infiltrates.
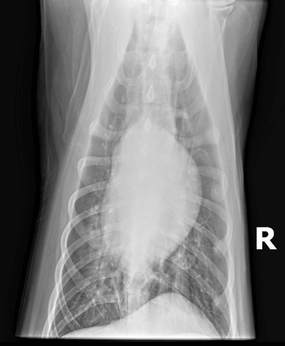 X-ray of a dog’s chest taken from a lateral view, displaying lung and heart structures with some notable infiltrates.
X-ray of a dog’s chest taken from a lateral view, displaying lung and heart structures with some notable infiltrates.
- Gastrointestinal Foreign Body by Jeremy Fleming, DVM, DACVS-SA - March 24, 2025
- Angular Limb Deformity by Russell Kalis, DVM, DACVS-SA - November 18, 2024
- Caustic Substance Injury by Jami Becker, DVM, DACVECC - September 30, 2024

