A 5-year-old spayed female Standard Poodle was brought to AVES ER with acute onset inappetence, teeth chattering, and intermittently turning left. After evaluation, the AVES ER team performed bloodwork, cervical/skull radiographs and a sedated oral examination which were unremarkable. She was started on carprofen and seemed to be improving. Three days later, she had her first seizure and was brought back to AVES for care. She was started on Keppra at this point.
Her physical examination was unremarkable. Her neurologic examination was performed during post ictal period and revealed multiple abnormalities including:
- Mentation: inappropriate
- Gait/Posture: mild tetraataxia
- Cranial Nerve Function: absent menace OU with intact visual tracking
- Postural Reactions: absent in both hind limbs, reduced in right forelimb
- Spinal Reflexes: intact x 4
- Epaxial Palpation: cervical pain
Inappropriate mentation, mild tetraataxia and absent menace OU were suspected to be post ictal changes. The asymmetry to the proprioceptive deficits (reduced RFL and normal LFL) and known seizure history localized patient to left forebrain. A concurrent cervical myelopathy could not be excluded due to her neck pain though referred pain from intracranial disease was suspected. Differential diagnoses included immune mediated meningoencephalitis, infectious meningoencephalitis and neoplasia.
A systemic workup was performed revealing the following results:
- Blood pressure: 156mmHg systolic
- PCV/TS: 47/8.2
- CBC: all values within reference interval
- Chemistry: all values within reference interval
- CXR: Unremarkable thoracic radiographs.
- UA: USG 1.016, WBC none, Bacteria – cocci/rods 51-100
- Urine culture: positive for Enterococcus sp., E.Coli and Enterobacter aerogenes
A neurologic diagnostic workup included both an MRI and CSF tap. Results of these diagnostics revealed:
- MRI: Moderate regional meningeal enhancement at the ventral aspects of the cerebrum and caudal fossa. Additionally, there is symmetrical enhancement of the ventral aspect of the hypothalamus. Differentials include meningoencephalitis (infectious or non-infectious) or neoplasia (such as round cell tumor).
- CSF: TP 105mg/dL (normal range <30); WBC 129/uL (normal range <5); cytology – moderate septic neutrophilic pleocytosis with bacterial rods present
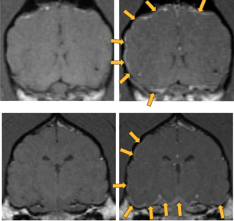
T1 precontrast images on left; post contrast images on right.
Arrows on post contract images point to predominantly left sided and ventral meningeal enhancement.
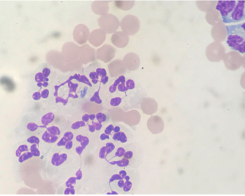
Image of non-degenerate neutrophils in the CSF with single neutrophil containing several long slender bacterial rods.
Following the MRI, the patient was empirically started on enrofloxacin due to concerns for bacterial meningitis.
We were unable to perform a CSF culture as there was not a sufficient sample. Because of concern for hematogenous spread of infection, blood and urines cultures were offered. Blood cultures were declined.
Urine culture confirmed the presence of E.Coli and Enterobacter which were both sensitive to enrofloxacin. Additionally, Enterococcus was also cultured which only had intermediate sensitivity to enrofloxacin therefore amoxicillin was added to the treatment regimen. Enrofloxacin was continued for 8 weeks and amoxicillin was only continued for 4 weeks due to the patient developing GI upset. Keppra was started due to her seizure on presentation.
The patient began improving within a few days of starting antibiotics and presented neurologically normal at her 4 week recheck. Her urine culture was negative after 8 weeks of treatment. She had no seizures after initiation of treatment. Keppra was tapered after 8 weeks with no seizures after discontinuation. The patient was clinically normal with no recurrent seizures at time of last recheck 6 months after initial onset.
- Management of Prolonged Starvation in a Cat –by Amaris Franco, DVM, DACVECC - June 13, 2024
- Canine Heat Stroke – by Jami Becker, DVM, DACVECC - May 20, 2024
- Bacterial Meningitis – by Tracy Sutton, DVM, DACVIM - January 29, 2024

