SIGNALMENT
13 week old, Female Intact, Labrador
HISTORY
On Monday Apri 17th around 1:30 pm Evie fell into her family’s pool. When she was pulled from the water she was weak, had a dull mentation and was having difficulty breathing. She was taken immediately to her primary care veterinarian where radiographs were performed, and she was then transferred to AVES for further care.
4/17 PERTINENT PHYSICAL EXAM FINDINGS:
T- 102.9 F, HR- 164 bpm, RR- 120 bpm
Respiratory system: severely dyspneic, orthopneic, increased bronchovesicular sounds bilaterally.
Cardiovascular: no murmur or arrythmia noted, strong synchronous pulses
Otherwise, no abnormal physical exam findings
4/17 DIAGNOSTICS:
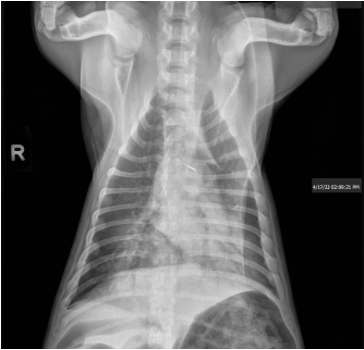
– 3 view chest radiographs performed at primary care veterinarian on 4/17/23:
- Severe symmetrical caudal dorsally distributed alveolar pulmonary infiltrates consistent with non cardiogenic pulmonary edema secondary to reported near drowning event.
- Subjective microcardia may represent hypovolemia.
- Gas filled stomach and small bowel consistent with aerophagia.
– CBC/Chemistry: no significant findings
– Arterial and venous blood gas was performed for comparison, however I suspect the arterial sample was actually venous blood since the values were identical, so this was not used to help determine treatment in this case.
4/17 CASE PROGRESSION
Initially Evie was placed in an oxygen cage at 60% O2 and administered a single dose of furosemide at 1 mg/kg IV, IV fluids at 60 ml/kg/day and unasyn in case of aspiration during drowning episode. She temporarily seemed to improve in the oxygen cage and was able to rest but after a couple of hours was awake, distressed, orthopneic and starting to show signs of fatigue. Evie’s owners were contacted and transitioning to high flow nasal oxygen therapy was recommended. Her initial high flow oxygen settings were FiO2 100%, air temperature 33 C, 0.8 L/kg.min oxygen flow. The oxygen flow rate was titrated up to 1.8 L/kg/min throughout the night. She remained dyspneic and orthopneic when aware and was kept calm with intermittent butorphanol.
4/18 CASE PROGRESSION
Her physical exam was static from 4/17. Due to stress/excitement and concern that it was worsening her respiratory status she was started on a butorphanol CRI at 0.1 mg/kg/hr which improved her comfort. The FiO2 of the high flow nasal oxygen was decreased to 80% with no worsening in her respiratory status. Overnight her respiratory stusu started to improve and she began breathing with only a slight increase in respiratory effort so the FiO2 was further weaned down to 40% and the oxygen flow rate was decreased to 1.3 L/kg/min.
4/19 CASE PROGRESSION AND OUTCOME
DIAGNOSIS
Non-cardiogenic pulmonary edema secondary to drowning.
HIGH FLOW NASAL OXYGEN THERAPY

- Provides warm and humidified oxygen up to an FiO2 of 100% and flow rate of 40 L/min.
- Decreases rebreathing and every breath contains the prescribed oxygen % and flow rate
- May provide positive airway pressure to help open up alveoli
- Provides heated and humidified air which improves patient comfort, prevents desiccation related tissue damage, helps mucociliary clearance
- Allows better patient access for critical patients vs being inside of an oxygen case
- Management of Prolonged Starvation in a Cat –by Amaris Franco, DVM, DACVECC - June 13, 2024
- Canine Heat Stroke – by Jami Becker, DVM, DACVECC - May 20, 2024
- Bacterial Meningitis – by Tracy Sutton, DVM, DACVIM - January 29, 2024

