Christy Corp-Minamiji, DVM
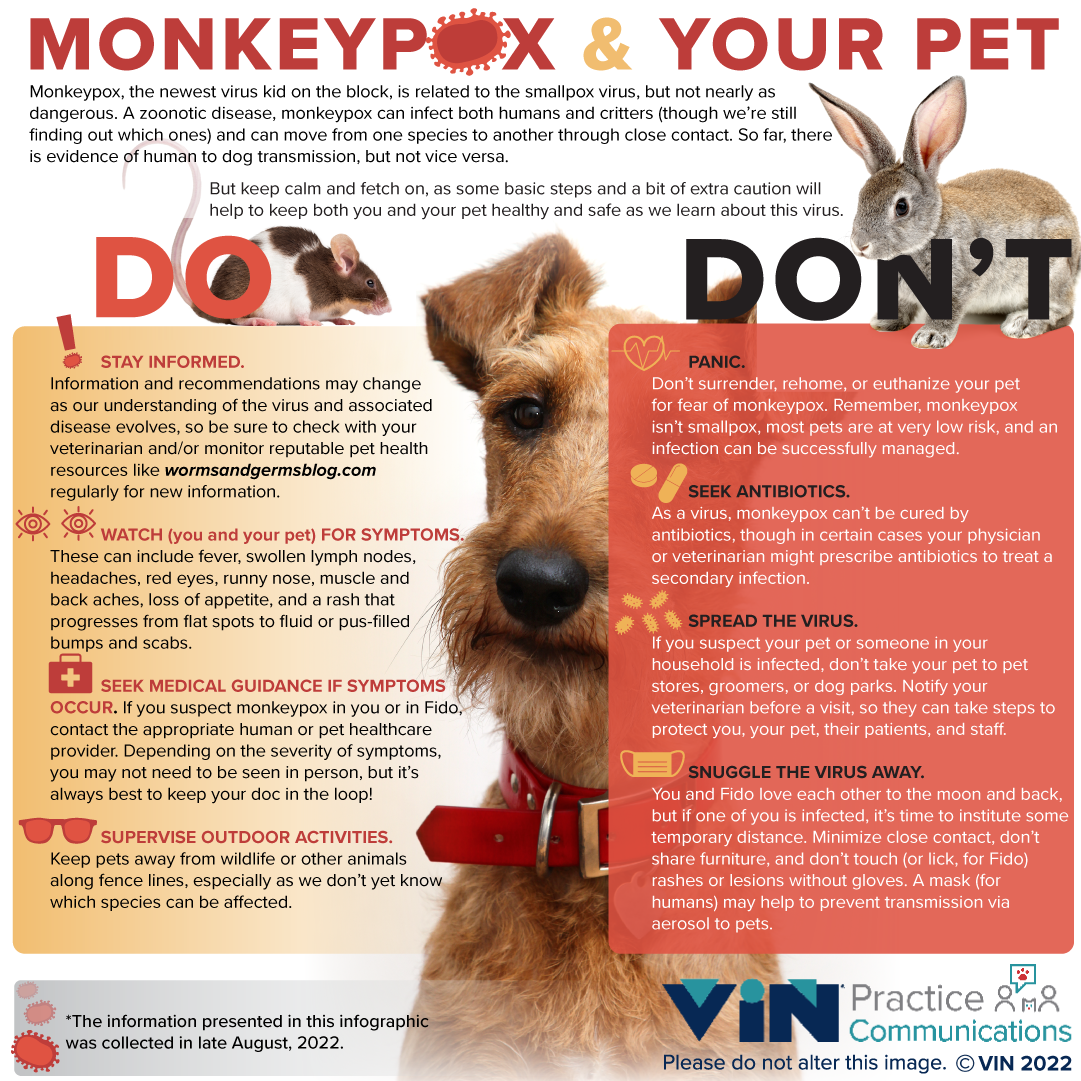
It seems like we barely figure out one new virus these days before another hits the news. You’ve almost certainly heard of the Monkeypox virus by now and have questions about your own health and that of your pets. While we’re still learning more about this virus and how it moves between different species of animals, here are some answers on how to keep your pets and your family healthy.
What Is Monkeypox?
Monkeypox is a disease caused by a virus related to the smallpox virus. However, it causes less severe illness and is far less likely to cause death than smallpox. Monkeypox is also a zoonotic disease. This means it can infect both humans and non-human animals and can move from one species to another. Because it is caused by a virus rather than bacteria, antibiotics won’t cure it, though in certain cases, your physician or veterinarian might prescribe antibiotics to treat a secondary infection.
Can My Pets Get Monkeypox?
We still don’t know all the species Monkeypox can infect. Right now, humans, non-human primates (monkeys, chimps, etc.), and certain rodents seem to be the most vulnerable. We do know that it can infect rabbits, mice, and dogs. The jury is still out on cats. It is a disease of mammals, so it’s unlikely to infect your birds, reptiles, amphibians, or fish. While we know humans can infect dogs, we aren’t yet sure if the reverse is true.
What Are the Symptoms?
In people, we know that Monkeypox can cause the following symptoms: fever, swollen lymph nodes (“glands”), headaches, red eyes, runny nose, muscle and back aches, loss of appetite, and a rash that progresses from flat spots to fluid or pus-filled bumps and scabs. We can’t know if our animal friends experience headaches, muscle, or backaches, but the rest of the signs appear to be the same in animals as in humans.
How Is Monkeypox Spread?
For the most part, Monkeypox appears to be spread through close contact such as direct contact with skin lesions, respiratory droplets (coughs, sneezes, kisses, licks, close breathing), and contact with contaminated surfaces that then enters the body through the eyes, mouth, or broken skin.
We do know that humans can become infected with Monkeypox from close contact with infected animals and vice versa. However, we don’t yet know exactly which animals can transmit to humans.
What Should We Do if We Think a Person or Pet in Our Home Has Monkeypox?
If any of the humans or pets in your home show the symptoms listed above or have been in close contact with another person or animal infected with Monkeypox, contact your veterinarian or physician or both right away.
Meanwhile, here are 10 steps you can take to reduce the potential for spread within your home if you, your pet, or someone you know has been exposed to Monkeypox:
- An infected person can wear a mask around pets and other humans.
- Clean and disinfect commonly touched surfaces regularly. Minimize close contact between infected pets and humans or other pets.
- Don’t kiss or allow close-face contact between pets and infected humans (or vice versa).
- Don’t allow pets on furniture used by infected humans.
- Don’t touch any rashes or skin lesions you see on your pet without gloves.
- Don’t take your pets to pet stores, groomers, or dog parks if you suspect exposure or infection.
- Supervise your pets in the yard to minimize contact with wildlife or other animals along fence lines.
- Don’t move your pet out of the household if it’s already exposed.
- Don’t surrender or euthanize your pet for fear of Monkeypox.
- If you need to take them to your veterinarian, let the office know that a member of your household has been exposed to or is infected with Monkeypox so the proper steps can be taken to make sure all patients and staff stay healthy.
– at a minimum,
What Else Should I Know?
Links to CDC and Worms and Germs blog:
https://www.cdc.gov/poxvirus/monkeypox/veterinarian/monkeypox-in-animals.html
- Gastrointestinal Foreign Body by Jeremy Fleming, DVM, DACVS-SA - March 24, 2025
- Angular Limb Deformity by Russell Kalis, DVM, DACVS-SA - November 18, 2024
- Caustic Substance Injury by Jami Becker, DVM, DACVECC - September 30, 2024

